Dietitian resources and FAQ’s
In this page you will find helpful dietitian resources and answers to frequently asked questions:
Food Diary
At the start of the program you will be asked to fill in a food diary, this allows us to work together to ensure an individualized approach with you. There is no one size fits all.
The above video provides some helpful information around filling in the food diary.
A food diary template can be found here Electronic Copy Food Diary
Post bariatric surgery advice
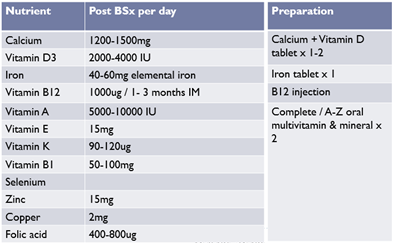
People who undergo bariatric surgery need to take vitamin and mineral supplements every day, lifelong, due to the increased risk of developing micronutrient deficiencies after bariatric surgery. Vitamin and mineral deficiencies can cause serious side effects, so it is important to take all the recommended supplements in order to avoid any problems.
Part of the preparation for bariatric surgery in the Centre for Obesity Management is understanding and agreeing to take lifelong vitamin and mineral supplements. Vitamin and mineral deficiencies can cause a range of serious side effects, but these can be avoided by taking the recommended supplements.
The following vitamin and mineral supplements are recommended:
- Complete multivitamin and mineral supplement (containing thiamine, iron, selenium, zinc, & copper)
- Iron
- Calcium with Vitamin D
- Intramuscular Vitamin B12
Your local pharmacy should stock the recommended supplements. Some types of iron, calcium with vitamin D and vitamin B12 injections are currently covered on the medical card in Ireland. Complete multivitamins are not, and tend to cost around 10-15 euro per month. It is important to consider this long-term cost before deciding to proceed with bariatric surgery.
How often you need to have blood tests of some vitamin or mineral levels checked varies, depending on the type of surgery, how long ago the surgery was performed, and if you are reporting any unexplained symptoms.
At a minimum the blood tests should be checked annually. You may need to talk to your GP to arrange a review that includes having these blood tests.
Your GP may find helpful information on this website page and the UK BOMSS GP Hub https://bomss.org/gp-hub/
ASOI Adult Obesity Clinical Practice Guideline adaptation (ASOI version 1, 2022) by: Rhynehart A, Collins C, Woods C. Bariatric Surgery: Postoperative Management, Chapter adapted from: Shiau J, Biertho L. Available from: https://asoi.info/guidelines/postop/ Accessed [14/03/2024]
British Obesity and Metabolic Surgery Society Guidelines on perioperative and postoperative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery (2020 update) by: O’Kane M, Parretti HM, Pinkney J, et al. Obesity Reviews. 2020; 21:e13087.
Obesity Management Medications
Different obesity medications effect food absorption and metabolism, increase fullness hormones, and reduce appetite. Orlistat (Xenical) is an oral medication that effects fat absorption. GLP-1 medications include Liraglutide (Victoza/Saxenda) and Semaglutide (Ozempic) which are daily or weekly injections which can reduce appetite and increasing feelings of fullness. Naltrexone/Bupropion (Mysimba) is another oral medication.
Medication | Orlistat (Xenical) | GLP1: Liraglutide (Victoza) / Semaglutide (Ozempic) | Naltrexone/ Bupropion (Mysimba) |
Common side effects
| Loose oily stools that are difficult to flush, wind | Feeling sick (nausea), constipation, vomiting, diarrhoea | Feeling sick (nausea), constipation, dry mouth, headache, dizziness, diarrhoea |
Medication | Orlistat (Xenical) | GLP1: Liraglutide (Victoza) / Semaglutide (Ozempic) | Naltrexone/ Bupropion (Mysimba) |
Dietary changes | • Avoid fatty foods e.g. fried food, oils, creamy sauces, butter, spreads, crisps, chocolate, cakes, cream, fatty meats etc. • Take a multivitamin 2 hours before / after the medication | • Nausea / diarrhoea: slower eating, regular meal pattern; reduce portion sizes; low fat foods • Constipation: increase fibre & fluid; consider a laxative | • Nausea: slower eating, regular meal pattern; reduce portion sizes; low fat foods • Constipation: increase fibre & fluid; consider a laxative • Dry mouth / dizziness: increase water |
Alongside healthy lifestyle behaviours, obesity management medications can help to improve health problems linked with higher body weight and increase weight loss. You will get the best response from these medications if you have a regular eating pattern, with protein, plenty of fibre and fluid throughout the day.
- Meal pattern: Aim for about 3 meals per day, with snacks in between meals if needed
- Balance: Include lots of vegetables / fruit + some protein (fish / meat / chicken / eggs / beans / milk / cheese / yoghurt / Quorn) + some high fibre grains (wholegrain bread / rice / pasta / cereal / potato with skin on) at each meal

- Fat: Avoid fried foods, fatty meats, high fat snacks, or adding a lot of butter or oils to meals
- Fluid: Aim for a minimum of 2 litres of water each day
- Portions: When you start a new medication it’s difficult to tell how much it will reduce appetite. Start by reducing portions by about 1/3 until you learn it’s effect on your appetite.
- Mindful eating: Eating slowly gives you time to get used to new feelings of fullness with medications. Taking time to plan your meals and focus on the enjoyable tastes and textures as you eat also helps.
