Bias and stigma
Weight bias refers to our attitudes and beliefs about obesity and people living in larger bodies. An example is if we believe that people with obesity are lazy or lacking in will power. These are our own negative views.
Weight Stigma refers to social stereotypes that are very deeply ingrained within society. Examples are stereotypes that people with obesity eat too much or that they don’t do enough exercise. This stigma is pervasive across many systems, including healthcare settings, schools, and workplaces.
Discrimination happens when we act on our biases or because of social stereotypes, and we treat people differently, treat people unfairly.
The driving force of stigma arises from the misconceptions and misunderstanding of the complex causes of obesity, with people attributing weight gain to personal responsibility and failing to grasp the complex mix of genetics, environment and biological factors.
Weight stigma can be external, it can come from our community, environment or experiences, however people may also experience internal weight bias – this is when a person’s own beliefs around their body or weight can impact the way they think or act. They hold negative beliefs against themselves. This has a significant negative impact on mental and physical health, and can contribute to further weight gain.
Weight bias and stigma is influenced by negative media representations of people living with obesity. The media portrayal of obesity is often stigmatising and inaccurate, but it is influential and insidiously impacts society stereotypes.
We all need to work together to End Weight Stigma. You can read and learn more here:
https://asoi.info/guidelines/weightbias/
Listen to Dr Jean O’Connell and ICPO advocate Ms Susie Birney discuss Obesity and Stigma on our HSE podcast
Obesity is a complex, multi-factorial, chronic disease, just like high blood pressure, asthma, heart failure and type 2 diabetes.
Below is an article written by Dr Jean O’Connell – It was first published on the ICPO website
Dr Jean O’Connell, Consultant Endocrinologist, St Columcille’s Hospital Centre for Obesity Management
Chronic Disease Management – why is obesity treated differently?
In order to effectively manage a patient with a chronic disease such as asthma, there are a range of inhaled and oral medications that are tailored to each patient’s disease requirements. But imagine if a patient with asthma was reporting shortness of breath, wheeze and cough, and their doctor was unable or unwilling to prescribe them any medication. The doctor said to them repeatedly – “you just need to breathe a bit slower”. When the patient’s symptoms didn’t improve, and in fact became worse, the doctor said that they would have to help themselves, because clearly they weren’t trying hard enough to breathe slowly. The doctor told the patient that a friend of theirs had the same problem a few years ago, with a cough and some wheeze, and just doing some breathing exercises, and breathing slowly, had really helped their friend. “You should try this too. If it worked for my friend it should also work for you”. The patient might leave the clinic thinking that this doctor was not listening to them, and not managing their disease effectively. But if their own doctor isn’t listening to them, the patient is not sure where else they can go to seek help and support.
Another good example of chronic disease management is treatment of high blood pressure (BP). We have over 11 different classes of BP medications. If one drug doesn’t lower BP sufficiently, we can add another one that works in a different way. In this way, it is uncommon for high BP not to be managed successfully. It sometimes requires 2-3 different medications, but effective BP control is very achievable. But imagine a situation where a patient is told by their doctor that their BP is too high. The doctor advises the patient to reduce salt, reduce alcohol intake, try not to work very long hours, and go for a walk 4-5 days per week. The patient comes back 2 months later having made these changes, but the BP is still too high. The doctor is unable or unwilling to prescribe any medication that might help, because the doctor thinks that the patient is probably just pretending they made the recommended changes, and thinks that the patient should have tried harder. The doctor is aware of one medication that can sometimes help lower BP, but the medication is not reimbursed on the medical card, and it is very expensive, so the patient couldn’t afford it anyway. Instead, the doctor tells the patient to reduce salt even more, and to walk every day, and to really try hard this time. “The next time I see you your blood pressure should have reduced by 20mmHg, or you’re just not trying hard enough”. The patient would most likely leave the clinic thinking that it is their own fault that they have high BP, and feel a sense of hopelessness that they could ever achieve what the doctor has recommended.
Health professionals are familiar with the principles of chronic disease management. We understand that it involves a collaborative, patient-centred, holistic approach, with support from a multi-disciplinary team, and regular medical review, in primary, secondary and/or tertiary care services, over the course of a patient’s life. In addition to advice about healthy behaviours, we usually have a broad range of medications to choose from, that focus on different aspects of the disease, so if one medication isn’t effective, there is a different medication to add in or try instead.
Obesity is a complex, multi-factorial, chronic disease, just like high blood pressure, asthma, heart failure and type 2 diabetes. But instead of managing obesity as a chronic disease, many doctors blame the patient for not losing weight, advise them they just need to try harder, or try a particular diet (because that worked for them, or a friend, or a different patient), or to exercise more.
Healthy behaviours are important in the management of all chronic diseases, but in many cases behaviour change alone will not be sufficient. Like many chronic diseases, obesity is caused by an underlying genetic predisposition, leading to biological and hormonal dysfunction of homeostatic mechanisms. This is associated with a range of positive and negative influences, such as individual psychology, physical activity and built environment, food production and consumption, and social, society and media influences. We do not judge other patients with chronic diseases, when their illness is complex and severe, and requires medical and multidisciplinary team support. Why is there so much judgement among health professionals, of patients who are living with the disease of obesity? Why are we not educated appropriately, about the wealth of scientific data, that not only explains the nature of obesity as a chronic disease, but clearly shows how experiences of stigma and bias in health care settings are associated with weight gain and poorer health outcomes? Many believe that the stigma may be a useful source of motivation, to encourage people with obesity to adopt healthier behaviours. In fact, the reverse is true. There is considerable evidence that exposure to weight stigma in adults and children, leads to increased caloric consumption and reduced motivation to exercise.
Obesity stigma is based on the misconception that obesity is a choice. This untruth has led to inadequate funding of obesity research, under-resourcing of weight management and bariatric clinical centres, a tiny pool of pharmacological treatment options, minimal training of health professionals in obesity management, and confusing and unhelpful public-health campaigns. Media and public-health messages often underplay the significant effort and commitment required to lose weight and not regain weight. We need to counteract this myth. We need to tell our patients that it is not their fault, that it is achievable but difficult to lose weight, and not uncommon to regain it. We need to focus more on health gains rather than weight loss. Obesity stigma is reinforced when we place the emphasis on volitional control of body weight, rather than the multiple genetic, biological and environmental factors. We all have a roll in relaying this message, to patients, our colleagues, our family and friends, the media, politicians and governmental agencies. Most people living with obesity will never achieve a so-called ‘normal’ weight. We have a responsibility to support people to achieve their best weight, and to help create a society that does not judge people at any weight.
https://icpobesity.org/are-we-managing-obesity-as-a-chronic-disease/
Below are some other resources around stigma;
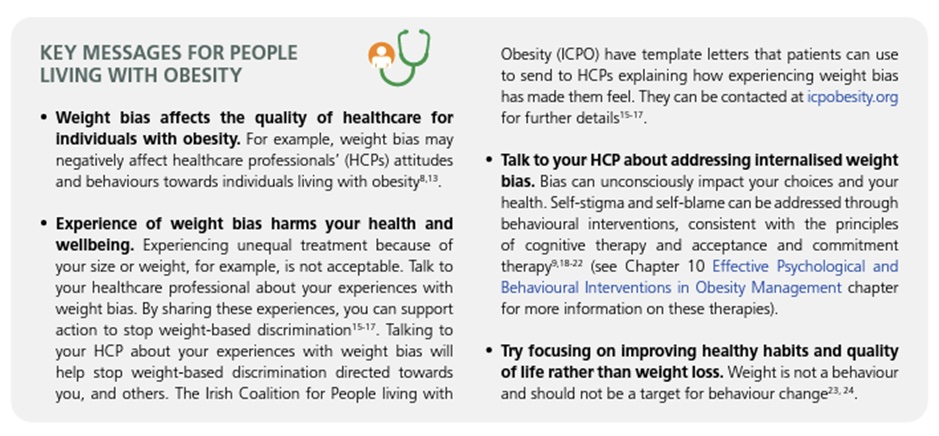
Key messages for people living with obesity taken from ‘ASOI Adult Obesity Clinical Practice Guideline adaptation (ASOI version 1, 2022) by: Heary C, Ryan L, Birney S, Arthurs N, O’Connell J. Reducing Weight Bias in Obesity Management, Practice and Policy, Chapter adapted from: Kirk SFL, Ramos Salas X, Alberga A, Russell-Mayhew S. Available from: https://asoi.info/guidelines/weightbias
